Demystifying Hypertension: A Nursing Concept Map Approach
Related Articles: Demystifying Hypertension: A Nursing Concept Map Approach
Introduction
In this auspicious occasion, we are delighted to delve into the intriguing topic related to Demystifying Hypertension: A Nursing Concept Map Approach. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
- 1 Related Articles: Demystifying Hypertension: A Nursing Concept Map Approach
- 2 Introduction
- 3 Demystifying Hypertension: A Nursing Concept Map Approach
- 3.1 Understanding the Essence of Nursing Concept Maps
- 3.2 Constructing a Nursing Concept Map for Hypertension: A Step-by-Step Guide
- 3.3 FAQs Regarding Nursing Concept Maps for Hypertension:
- 3.4 Tips for Effective Nursing Concept Map Use:
- 3.5 Conclusion:
- 4 Closure
Demystifying Hypertension: A Nursing Concept Map Approach
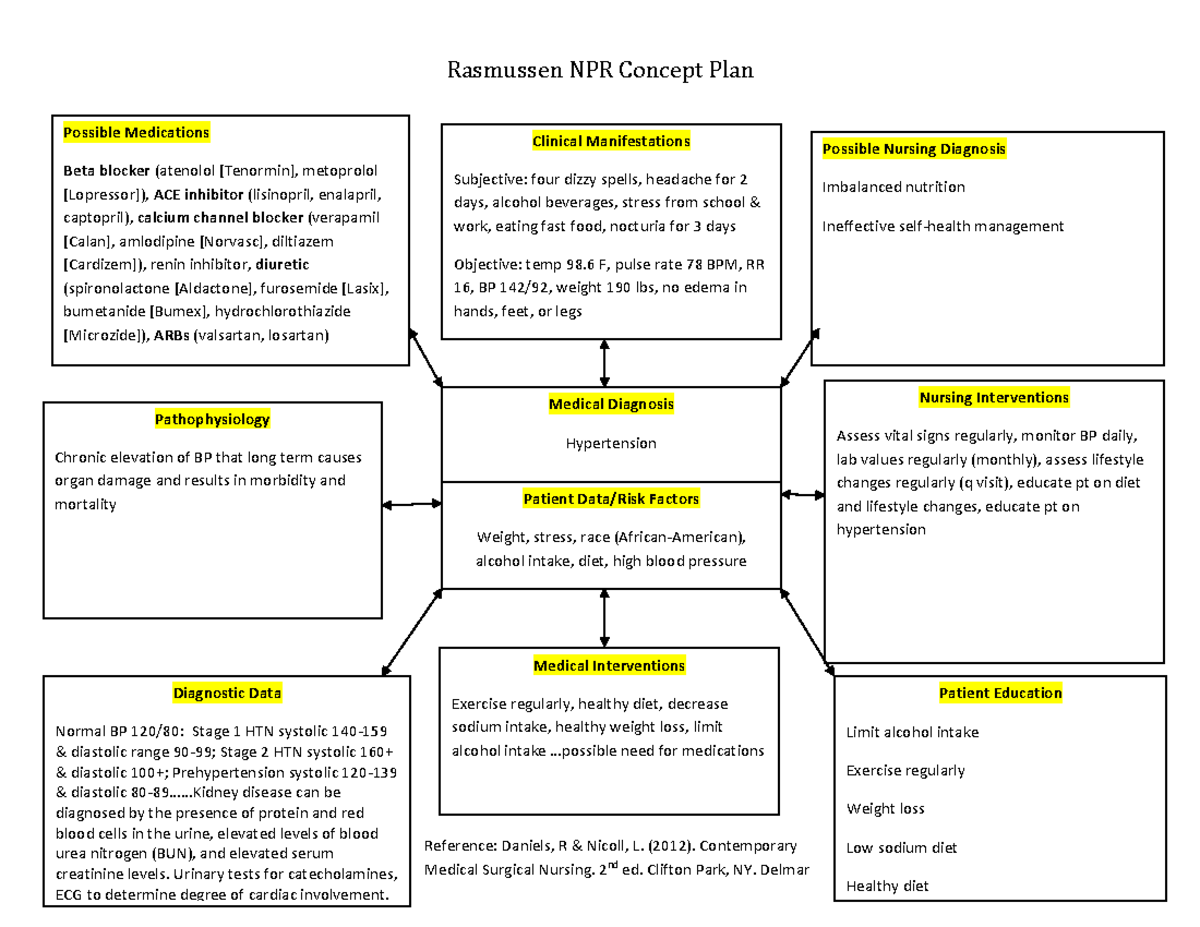
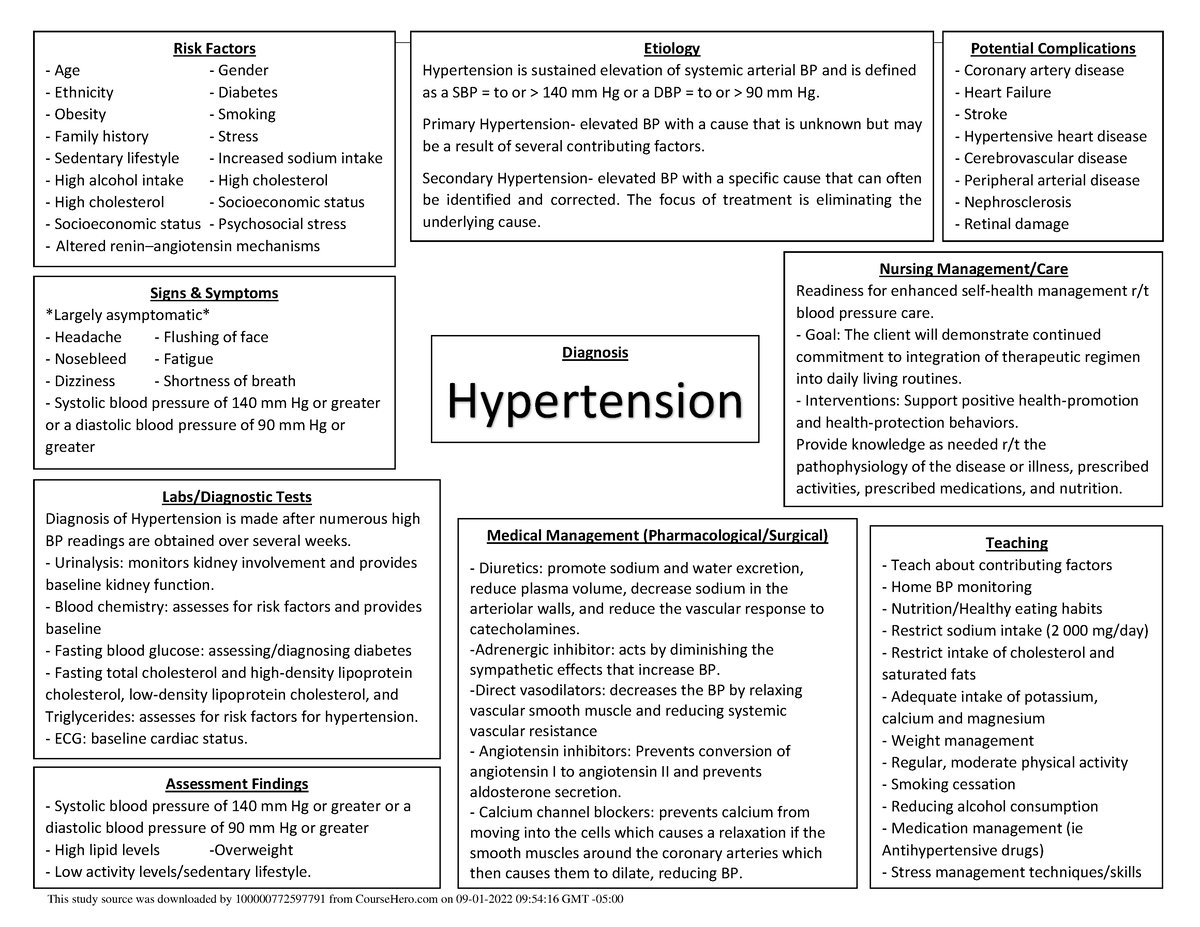
Hypertension, commonly known as high blood pressure, is a silent but pervasive health concern affecting millions globally. It is a significant risk factor for cardiovascular diseases, including heart attacks, strokes, and heart failure. Managing hypertension requires a multifaceted approach, encompassing lifestyle modifications, medication adherence, and ongoing monitoring. Nurses play a crucial role in this process, providing education, support, and individualized care plans. To facilitate a comprehensive understanding of hypertension management, nursing concept maps serve as valuable tools.
Understanding the Essence of Nursing Concept Maps
A nursing concept map is a visual representation of patient-specific information, outlining key concepts, relationships, and interventions. It serves as a dynamic roadmap for nurses, guiding their assessment, planning, implementation, and evaluation of care. In the context of hypertension, a nursing concept map helps to:
- Visualize the complexity of the condition: Hypertension is not merely a single diagnosis but a constellation of factors influencing its development and management. A concept map captures the interplay of physiological, psychological, and social aspects, providing a holistic perspective.
- Identify individual patient needs: Each patient presents with unique risk factors, symptoms, and responses to treatment. A concept map facilitates a personalized approach, tailoring interventions to the specific needs and circumstances of the individual.
- Promote effective communication: The visual nature of a concept map fosters clear and concise communication among healthcare providers, ensuring consistency in care and avoiding redundancies.
- Facilitate critical thinking and problem-solving: The concept map encourages nurses to analyze data, identify patterns, and formulate appropriate nursing diagnoses and interventions. It fosters a proactive and evidence-based approach to care.
Constructing a Nursing Concept Map for Hypertension: A Step-by-Step Guide
Creating a comprehensive nursing concept map for hypertension involves several key steps:
1. Gathering Patient Data:
- Assessment: This encompasses collecting essential data from the patient, including medical history, current medications, family history of hypertension, lifestyle factors, and psychosocial considerations.
- Physical Examination: Vital signs, such as blood pressure, heart rate, and respiratory rate, are crucial. Other physical assessments may include examining for signs of target organ damage, such as retinopathy or hypertensive heart disease.
- Laboratory Tests: Blood tests, such as electrolytes, creatinine, and lipid profile, provide valuable insights into the patient’s overall health and risk factors.
2. Identifying Key Concepts:
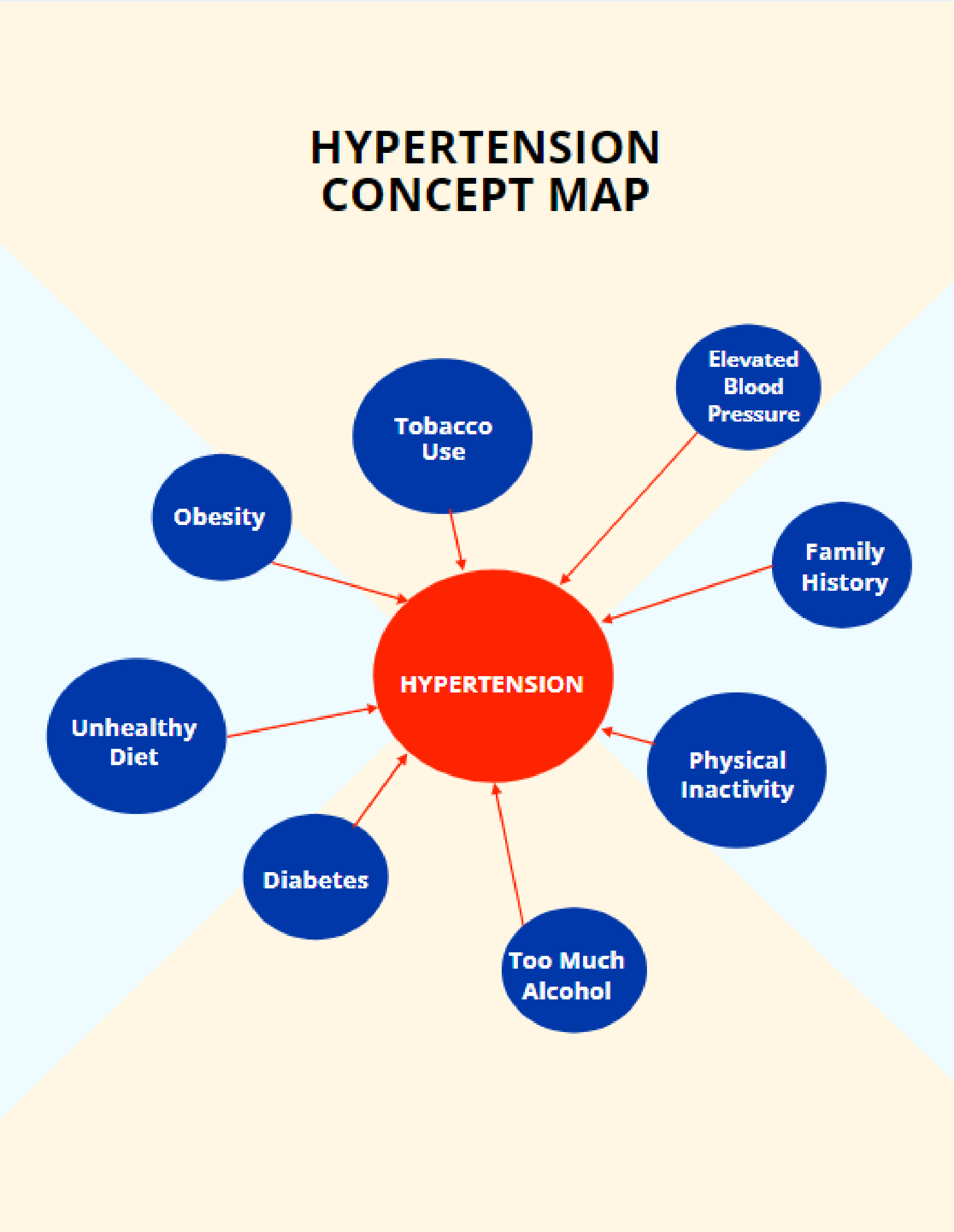
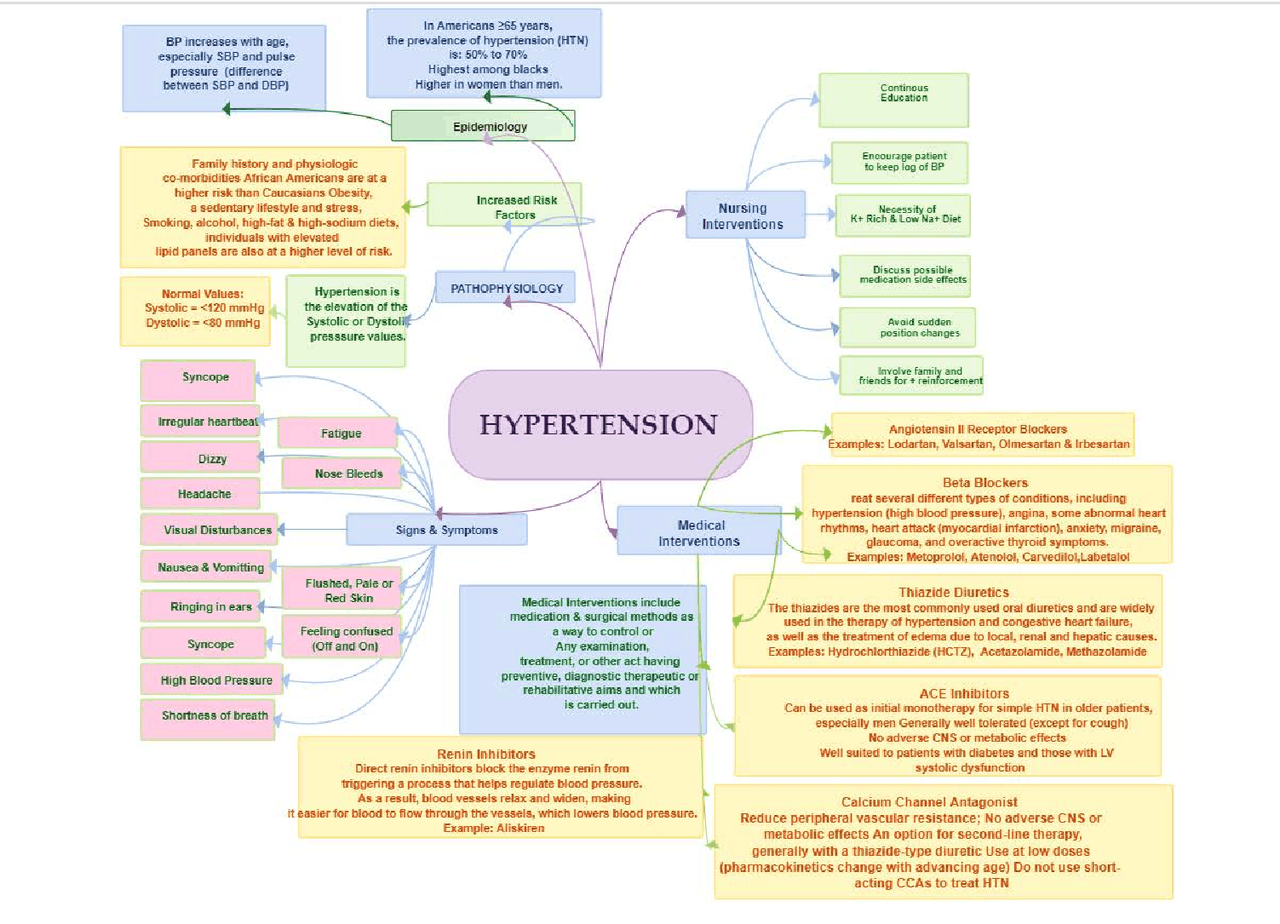
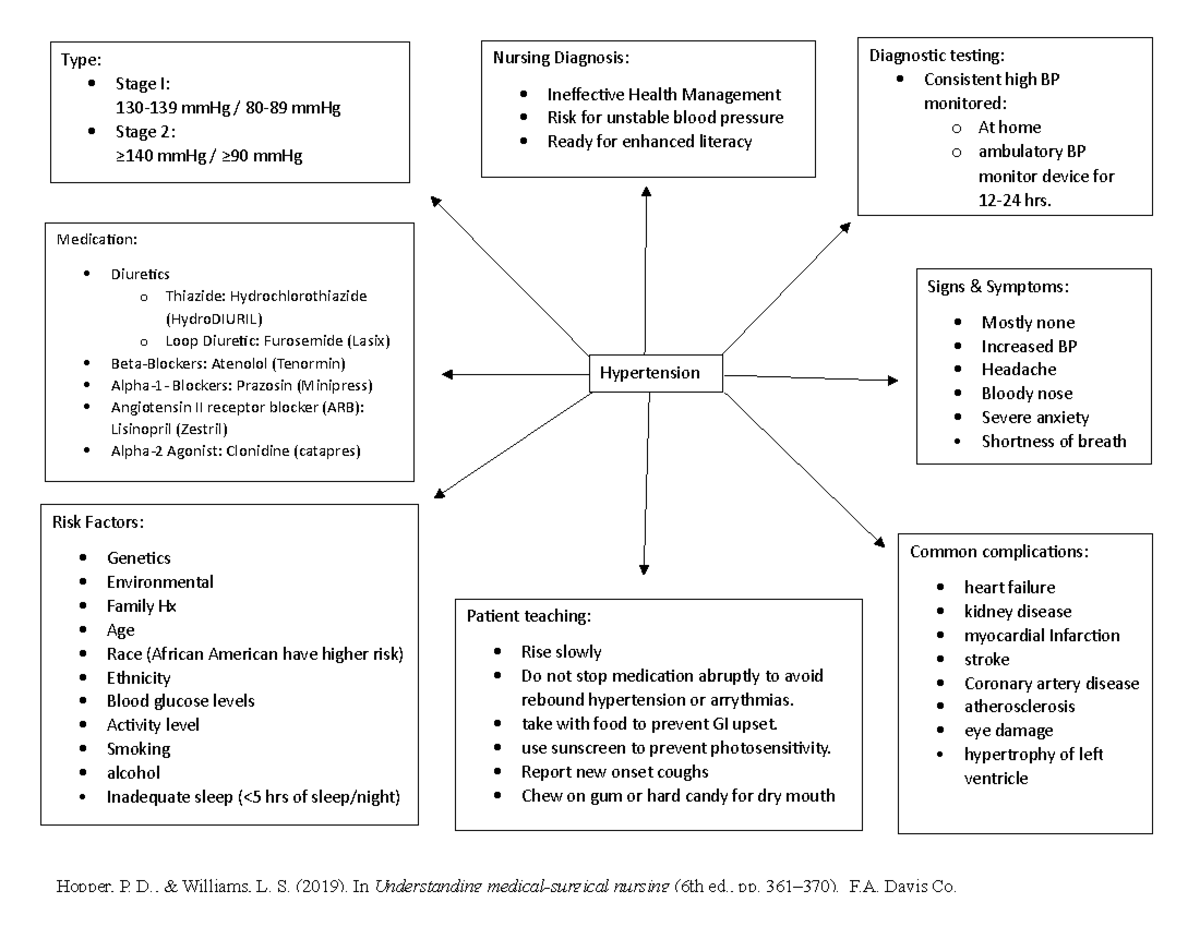
- Physiological: This includes the pathophysiology of hypertension, the mechanisms of action of antihypertensive medications, and the potential complications of uncontrolled hypertension.
- Psychological: Addressing the patient’s emotional response to the diagnosis, coping mechanisms, and adherence to treatment plans is crucial.
- Social: Factors like socioeconomic status, access to healthcare, and social support systems can influence a patient’s ability to manage hypertension effectively.
3. Establishing Relationships Between Concepts:
- Risk factors: Identify and analyze the patient’s specific risk factors for hypertension, such as age, race, family history, smoking, alcohol consumption, and obesity.
- Symptoms: Assess the patient’s presenting symptoms, such as headaches, dizziness, nosebleeds, and vision changes.
- Complications: Recognize potential complications associated with uncontrolled hypertension, including stroke, heart attack, kidney failure, and retinopathy.
4. Defining Nursing Diagnoses:
- Ineffective Management of Therapeutic Regimen: This diagnosis addresses the patient’s inability to adhere to prescribed medications or lifestyle modifications.
- Risk for Decreased Cardiac Output: Recognizing the potential for reduced heart function due to hypertension and its complications.
- Risk for Ineffective Peripheral Tissue Perfusion: Assessing the risk of impaired blood flow to extremities due to hypertension-related vascular damage.
5. Developing Nursing Interventions:
- Education: Provide comprehensive education on hypertension, including its causes, risk factors, treatment options, and importance of lifestyle modifications.
- Medication Administration: Ensure accurate and timely administration of prescribed antihypertensive medications.
- Lifestyle Modifications: Encourage and support the patient in adopting healthy lifestyle changes, such as weight management, regular physical activity, stress reduction techniques, and dietary adjustments.
- Monitoring: Regularly assess blood pressure and monitor for signs and symptoms of complications.
- Referral: Refer patients to other healthcare professionals, such as cardiologists, dietitians, or mental health specialists, as needed.
6. Evaluating Outcomes:
- Blood Pressure Control: Monitor blood pressure readings to assess the effectiveness of interventions and medication.
- Symptom Management: Evaluate the patient’s experience with symptoms, such as headaches or dizziness, to assess improvement.
- Adherence to Treatment: Assess the patient’s adherence to medication regimens and lifestyle modifications.
- Patient Satisfaction: Evaluate the patient’s satisfaction with the care provided and their understanding of the condition.
7. Reassessment and Revision:
- Regularly review the concept map: Update the map based on ongoing assessments, changes in the patient’s condition, and new information.
- Adapt interventions: Adjust the care plan as needed based on the patient’s response to interventions and progress towards goals.
FAQs Regarding Nursing Concept Maps for Hypertension:
1. What are the benefits of using a nursing concept map for hypertension?
Nursing concept maps enhance the quality of care by providing a comprehensive and individualized approach to hypertension management. They facilitate effective communication, promote critical thinking, and ensure continuity of care.
2. How often should a nursing concept map be reviewed and updated?
The frequency of review and update depends on the patient’s condition and the complexity of their care. Generally, it is recommended to review the concept map at least once a week or more frequently if there are significant changes in the patient’s status.
3. Can a nursing concept map be used for other chronic conditions?
Yes, nursing concept maps are a versatile tool applicable to a wide range of chronic conditions, including diabetes, heart failure, and chronic obstructive pulmonary disease.
4. What are some common challenges associated with using nursing concept maps?
Challenges may include the time required for initial development, the potential for complexity, and the need for ongoing maintenance. However, the benefits of using a concept map outweigh these challenges.
5. Are there any specific software programs or resources available for creating nursing concept maps?
Various software programs and online resources are available, such as ConceptDraw, MindManager, and Lucidchart. Some healthcare institutions also have their own internal systems for creating and managing concept maps.
Tips for Effective Nursing Concept Map Use:
- Keep it concise and relevant: Focus on the most essential concepts and relationships, avoiding unnecessary details.
- Use clear and consistent language: Ensure all terms and abbreviations are understood by all involved parties.
- Utilize visual aids: Incorporate diagrams, symbols, and color coding to enhance clarity and visual appeal.
- Collaborate with other healthcare professionals: Involve other members of the healthcare team, such as physicians, pharmacists, and social workers, in the development and review of the concept map.
- Regularly review and update: Ensure the concept map remains accurate and relevant to the patient’s current needs and condition.
Conclusion:
Nursing concept maps are invaluable tools for managing hypertension, promoting a comprehensive and individualized approach to care. By visualizing the complexity of the condition, identifying individual patient needs, and facilitating effective communication, they empower nurses to deliver high-quality, patient-centered care. Through careful construction, ongoing review, and collaborative effort, nursing concept maps can contribute significantly to improving outcomes for patients with hypertension.


Closure
Thus, we hope this article has provided valuable insights into Demystifying Hypertension: A Nursing Concept Map Approach. We appreciate your attention to our article. See you in our next article!